“Norovirus Surge in the U.S.: What You Need to Know About the Winter Outbreak”
As winter sets in, the United States is facing a significant surge in norovirus cases, a highly contagious stomach virus that causes severe gastrointestinal illness. Health experts are sounding the alarm about the increase in outbreaks across the country, with the Centers for Disease Control and Prevention (CDC) confirming a spike in norovirus-related incidents in recent weeks. With an alarming rise in cases, public health officials are urging the public to take precautions as the virus spreads rapidly through food sources, community settings, and even social gatherings.
What is Norovirus?
Norovirus is a highly contagious virus that causes inflammation of the stomach and intestines, leading to symptoms like nausea, vomiting, diarrhea, and stomach cramps. It spreads primarily through contaminated food or water, close contact with infected individuals, and surfaces contaminated by the virus. A person can contract norovirus by ingesting as few as 10 viral particles, making it incredibly easy to transmit.
The virus is responsible for an estimated 20 million cases of acute gastroenteritis annually in the U.S., according to the CDC. Norovirus is particularly troublesome because it can spread quickly in environments such as schools, nursing homes, and hospitals. The illness typically resolves within one to three days, but in some cases, particularly among vulnerable populations, complications like dehydration can lead to hospitalization or death.
The Surge in Outbreaks:
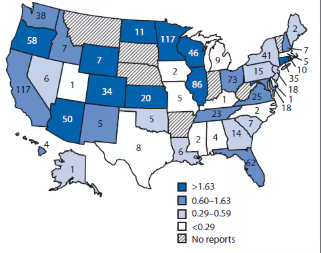
The recent surge in norovirus cases across the United States is of particular concern as the country enters the height of the winter season. Health officials reported 91 outbreaks during the week of December 5th, a notable rise from the 69 outbreaks reported just the week before. Experts attribute this surge to several factors, including the winter season when the virus thrives, and the holiday season when people gather in large numbers, increasing the potential for exposure.
In the past month alone, several significant outbreaks have been reported in various parts of the country, affecting thousands of individuals.
High-Profile Outbreaks and Incidents:
1. Seafood Contaminations:
One of the primary sources of the recent outbreak has been contaminated shellfish. On December 15th, the U.S. Food and Drug Administration (FDA) issued a recall for Manila clams and oysters harvested by Rudy’s Shellfish and S&M Shellfish Co. between November 15 and December 11. The oysters and clams were distributed across multiple states, including Arizona, California, and New York. These shellfish products were linked to a number of norovirus outbreaks, resulting in numerous illnesses. The FDA recommended that consumers immediately discard the recalled shellfish and seek medical attention if they exhibit symptoms like vomiting, diarrhea, or stomach cramps.
Health experts warn that people consuming raw oysters and clams are particularly at risk of contracting norovirus, as the virus can survive in the seafood even after it has been harvested.
2. Los Angeles Times Event:
A particularly alarming incident occurred during the Los Angeles Times’ “101 Best Restaurants” event on December 3rd, where over 80 attendees fell ill after consuming raw oysters linked to a norovirus outbreak. The oysters, supplied by Santa Monica Seafood, were identified as the source of the infection. Guests at the event experienced symptoms such as nausea, vomiting, and diarrhea shortly after eating the oysters. The Los Angeles County Department of Public Health has since launched an investigation to determine how the shellfish became contaminated, and the event organizers have issued an apology to those affected.
This outbreak highlights how easily norovirus can spread, even in controlled environments such as catered events. Health authorities are urging event organizers to ensure that food is sourced from reliable suppliers and properly prepared to avoid such outbreaks.
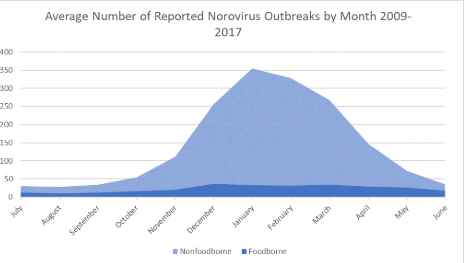
The Winter Spike in Cases:
Norovirus outbreaks are more common in the colder months, typically from November through April. During this time, the virus thrives in closed environments, where people are more likely to gather indoors. The flu season also coincides with norovirus outbreaks, which can make it difficult to differentiate between the two viral infections. Symptoms of both illnesses overlap, making it essential for individuals to seek medical advice if they exhibit signs of either virus.
The contagious nature of norovirus makes it challenging to contain, particularly in environments like cruise ships, schools, nursing homes, and restaurants, where close contact is unavoidable. The CDC has emphasized the importance of practicing strict hygiene and food safety measures to prevent outbreaks from spreading further.
Preventive Measures:
Given the highly contagious nature of norovirus, health experts recommend several steps individuals can take to protect themselves and others from the virus:
- Hand Hygiene: One of the most effective ways to prevent norovirus infection is frequent and thorough handwashing with soap and water, particularly before eating or preparing food and after using the restroom. Alcohol-based hand sanitizers are not effective in killing the virus.
- Disinfection: Norovirus can survive on surfaces for days, so cleaning and disinfecting frequently touched surfaces (such as doorknobs, countertops, and bathroom facilities) is essential, particularly in public places.
- Food Safety: Ensuring that seafood is sourced from reputable suppliers and properly cooked can help prevent contamination. Consumers should avoid eating raw oysters or shellfish from unverified sources, as these are often linked to norovirus outbreaks.
- Stay Home When Ill: Individuals exhibiting symptoms of norovirus should avoid preparing food for others and stay home to prevent spreading the virus. Those with symptoms should wait at least 48 hours after recovery before returning to public places or returning to work.
Impact on Vulnerable Populations:
While anyone can catch norovirus, certain groups are at greater risk of severe illness. Young children, the elderly, and individuals with weakened immune systems are particularly vulnerable to dehydration caused by vomiting and diarrhea. These groups may require medical attention to avoid complications.
Nursing homes and long-term care facilities are particularly susceptible to norovirus outbreaks, as residents often live in close quarters and share communal spaces. Outbreaks in these facilities can spread rapidly and have serious consequences for residents, who may be more vulnerable to dehydration and other complications.
Conclusion:
As norovirus cases continue to rise, public health officials are urging everyone to take preventative measures seriously. While norovirus typically resolves on its own within a few days, the rapid spread and severe symptoms it causes make it a significant public health concern.